Study: Hormonal birth control may reduce ovarian cancer risk in people with BRCA mutations
Summary
Hormonal birth control pill is linked to reduced ovarian cancer among people with an inherited BRCA mutation. Longer-acting forms of birth control given by implant, injection or as an intrauterine device may be associated with lower ovarian cancer risk for people with an inherited BRCA mutation. (Posted 4/28/23)
Este artículo está disponible en español.
Printer Friendly Page Read the Original Article
RELEVANCE
Most relevant for: Women with BRCA1 or BRCA2 mutations who are interested in reducing their ovarian cancer risk.
It may also be relevant for:
- people with a family history of cancer
- previvors
- people with a genetic mutation linked to cancer risk
Relevance: Medium-High


Strength of Science: Medium


Research Timeline: Human Research


What is this study about?
Researchers wanted to know how the use of long-acting birth control impacts ovarian cancer risk for people with an in or genes.
Why is this study important?
People with an inherited or mutation are at high risk for ovarian cancer. Research has shown that birth control pills decrease ovarian cancer risk for people at high risk, as well as everyone else.
Increased use of intrauterine devices (IUDs), birth control implants under the skin and injections has significantly reduced the use of birth control pills in the US. Birth control methods that do not require remembering to take a daily pill are associated with fewer unintended pregnancies but their effects on ovarian cancer risk were not known.
This is the first study to see if these long-acting forms of birth control reduce ovarian cancer risk in people with a mutation.
Hormonal birth control
Hormonal forms of birth control are medicines or devices that can reduce your risk of getting pregnant. Some forms of hormonal birth control contain a combination of the hormones and , while others contain only . Birth control pills (“the pill”), skin patches and a birth control ring that fits into the vagina are examples of hormonal birth control that contain both and . Progestin-only methods include pills, shots, implants that are placed under the skin and devices that are inserted into the uterus (intrauterine devices, also called IUDs).
Study findings
Hormonal birth control was linked to reduced ovarian cancer.
- Among women who used any type of hormonal birth control, the risk of ovarian cancer was reduced by 38% compared to women who never used hormonal birth control.
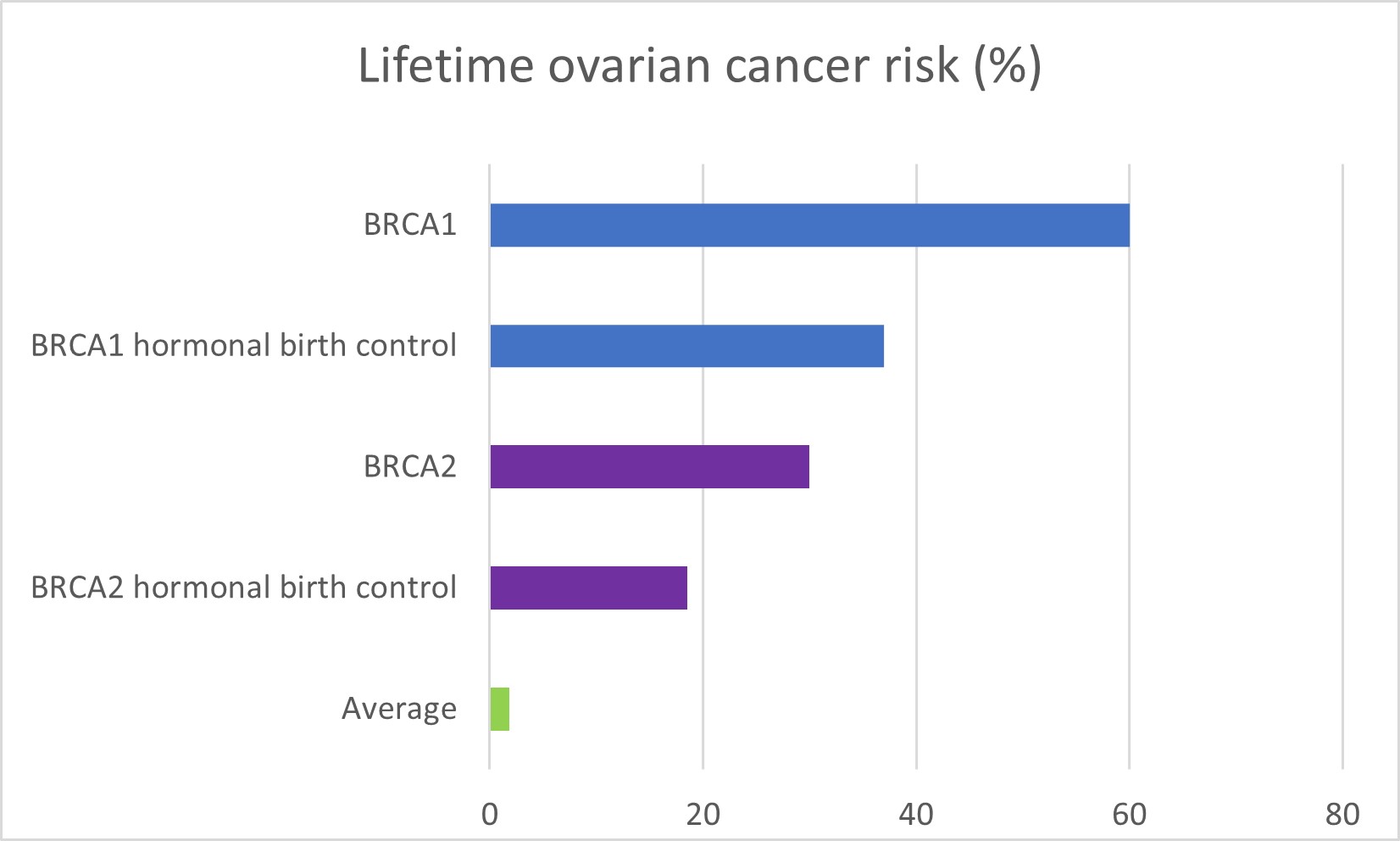
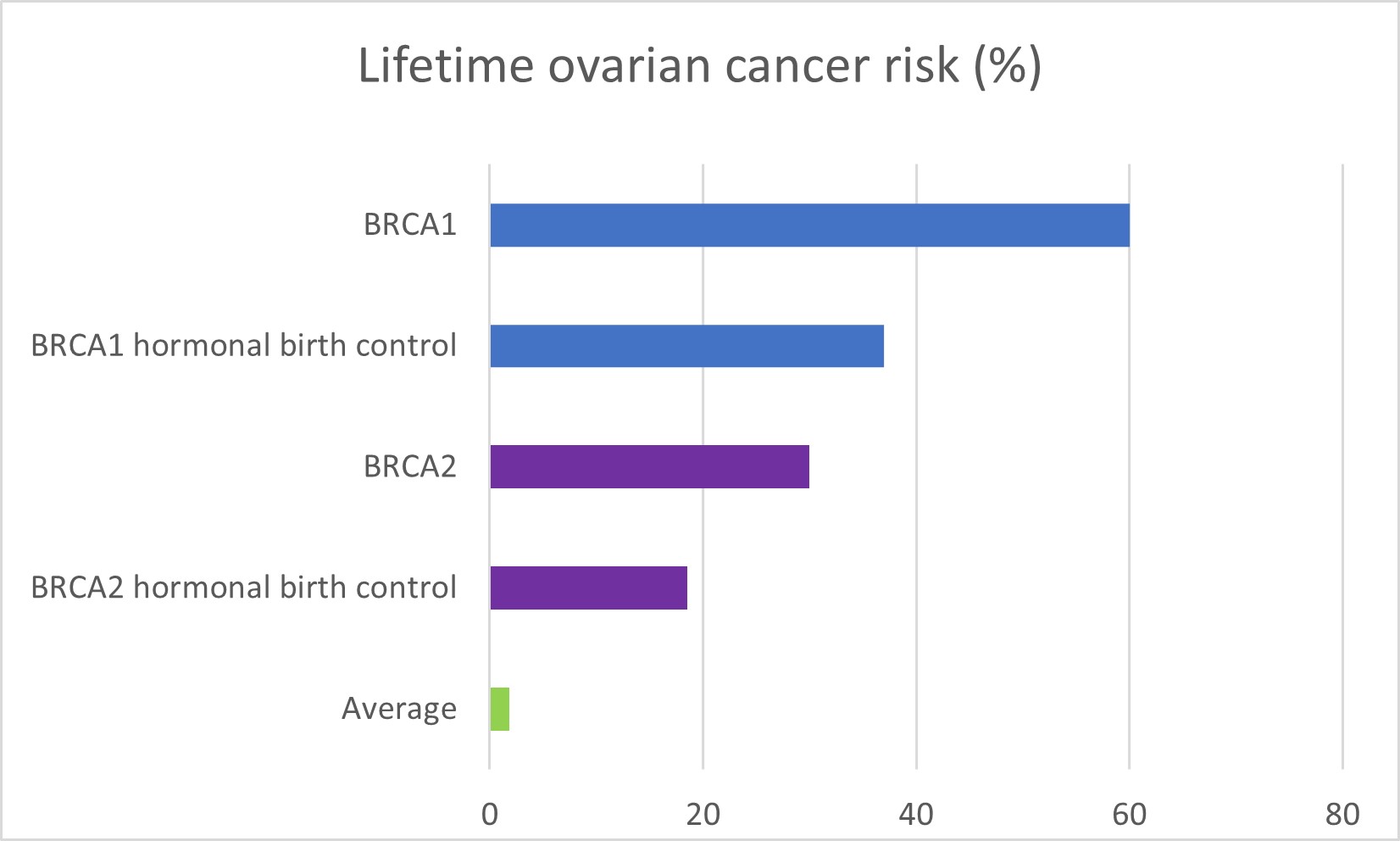
Differences in lifetime ovarian cancer risk based on mutation and use of hormonal birth control
- People who took birth control bills had reduced ovarian cancer.
- The use of birth control pills reduced ovarian cancer risk by 34%.
- This was statistically significant.
- This reduction in risk is similar to the results of other studies.
- The use of birth control pills reduced ovarian cancer risk by 34%.
- People using longer acting birth control (implants, injections or IUDs) tended to have ovarian cancer less often but this was not statistically significant.
- The use of implants reduced ovarian cancer risk by 70%.
- This was not statistically significant. This may be because only a few people in the study used implants (30 of 1741)
- The use of injections reduced ovarian cancer risk by 63%.
- This was not statistically significant. This may be because only a few people in the study used injections (12 of 1741).
- IUD use was associated with a small reduction in ovarian cancer risk.
- This finding was not statistically significant. This may be because only a few people in the study used IUDs (64 of 1741).
- The use of implants reduced ovarian cancer risk by 70%.
Participants who did not develop ovarian cancer were more likely to:
- have breastfed their children. This agrees with other research we covered in this XRAY review.
- have slightly more children (on average).
- have had a tubal ligation (had their tubes tied).
Risks from birth control:
Most women do not have serious side effects from hormonal birth control. Side effects may include:
- weight gain
- headaches
- sore breasts
- irregular periods
- mood changes
- decreased sexual desire
- acne
- nausea
Some types of hormonal contraception are more likely to cause certain side effects than others.
What does this mean for me?
If you have a or mutation, hormonal birth control may reduce your risk of ovarian cancer.
If you are considering using birth control to decrease your ovarian cancer risk, the information from this study may be useful in making decisions about the type of birth control you choose. Birth control pills were linked to reduced ovarian cancer. Longer-acting birth control methods (implants, injections or IUDs) tended to show reduced ovarian cancer but this was not statistically significant (maybe because few people in this study used these types of birth control). More research is needed to clarify if the use of long-acting contraception reduces ovarian cancer risk.
Reference
Xia Y, Gronwald J, Karlan B, et al., Contraceptive use and the risk of ovarian cancer among women with a or mutation. Gynecologic Oncology; 2022; 164(3):514-521.
Disclosure: FORCE receives funding from industry sponsors, including companies that manufacture cancer drugs, tests and devices. All XRAYS articles are written independently of any sponsor and are reviewed by members of our Scientific Advisory Board prior to publication to assure scientific integrity.
Share your thoughts on this XRAY review by taking our brief survey.
posted 4/28/23
The National Comprehensive Cancer Network (NCCN) provides guidelines for management of gynecologic cancer risk in people with and mutations.
Prevention
- Risk-reducing removal of ovaries and , (known as salpingo-oophorectomy) is recommended between ages 35-40 for and 40-45 for and upon completion of childbearing.
- Research studies show that removing the ovaries can increase survival for women with mutations.
- Women should talk with their doctors about the effects of early menopause and options for managing them.
- Women should talk with their doctors about the risks and benefits of keeping or removing their uterus (hysterectomy), including:
- Women with a mutation have an increased risk for a rare form of aggressive uterine cancer; hysterectomy removes this risk.
- For women considering hormone replacement after surgery, the presence or absence of a uterus can affect the choice of hormones used.
- Estrogen-only hormone replacement is less likely to increase the risk for breast cancer, although it increases the risk for uterine cancer. Women who still have their uterus are typically given hormone replacement with both and progesterone.
- Adding progesterone to hormone replacement can protect against uterine cancer. However, the combination of these hormones may increase the risk for breast cancer more than alone.
- A medical history of fibroids or other uterine or cervical issues may justify a hysterectomy.
- Oral contraceptives (birth control pills) have been shown to lower the risk for ovarian cancer in women with mutations. Research on the effect of oral contraceptives on breast cancer risk has been mixed. Women should discuss the benefits and risks of oral contraceptives for lowering ovarian cancer risk with their doctors.
- Removal of the only () is being studied as an option for lowering risk in high-risk women who are not ready to remove their ovaries. Studies on the effects of are ongoing. At this time whether lowers the risk for ovarian cancer in high-risk women remains unknown.
- Consider enrolling in a research study looking at this procedure to lower cancer risk.
Screening
- There are no proven benefits to routine ovarian cancer screening using transvaginal and a blood test. However, some doctors still recommend this screening, starting at ages 30-35.
- Women should be aware of the symptoms of gynecologic cancer and report abnormalities to their doctors.
Updated: 05/08/2024
The following are studies looking at ovarian cancer screening or prevention.
- NCT04251052: A Study to Compare Two Surgical Procedures in Women with Mutations to Assess Reduced Risk of Ovarian Cancer (SOROCk). This study is looking at whether women with mutations who remove just the can reduce the risk of ovarian cancer nearly as much as women who remove their ovaries and .
- NCT05287451: Risk Reducing With Delayed as an Alternative to Risk- Reducing Salpingo-oophorectomy in High Risk-Women to Assess the Safety of Prevention. This study will look at outcomes in women with , , , and who remove their , followed by removal of their ovaries compared to women who undergo standard-of-care removal of their ovaries and at the same time.
- Validating a Blood Test for Early Ovarian Cancer Detection in High-risk Women and Families: MicroRNA Detection Study (MiDE). The goal of MiDe is to develop a test to detect early-onset ovarian cancer. Currently, no reliable screening or early detection tests are available. Participants can be expected to provide up to 4 tubes of blood every 6 months for up to 5 years. These samples can be collected by mobile phlebotomy all around the US.
- NCT04794322: Developing a Test for the Detection of Ovarian Cancer. This study aims to develop an ovarian cancer early detection test that looks at found in a uterine (womb) washing and proteins found in the blood. Participants will not receive the results of their tests.
Additional clinical trials for ovarian cancer screening and prevention may be found here.
Updated: 09/11/2022
Study findings
This study included 3,466 participants. Researchers compared birth control use among participants with a or mutation who were diagnosed with ovarian cancer (1,733 cases) to those with a or mutation who had never had ovarian cancer (1,733 controls).
Among all participants, 1,741 used some form of hormonal birth control. Most (97%) took birth control pills:
- 1,687 took birth control pills.
- 64 women used any type of IUD for birth control. 48 used hormonal IUD.
- 30 women used an implant for birth control.
- 12 women used injections for birth control.
Hormonal birth control was linked to reduced ovarian cancer.
- Among women who used any type of hormonal birth control, the risk of ovarian cancer was reduced by 38% compared to women who never used hormonal birth control.
Projected change in lifetime ovarian cancer risk with a 38% reduction in lifetime risk is shown in the graph below.
- People who took birth control bills had reduced ovarian cancer.
- The use of birth control pills reduced ovarian cancer risk by 34%.
- This was statistically significant.
- This reduction in risk is similar to the results of other studies.
- The use of birth control pills reduced ovarian cancer risk by 34%.
- People using longer acting birth control (implants, injections or IUDs) tended to have ovarian cancer less often but this was not statistically significant.
- The use of implants reduced ovarian cancer risk by 70%.
- This was not statistically significant. This may be because only a few people in the study used implants (30 of 1741)
- The use of injections reduced ovarian cancer risk by 63%.
- This was not statistically significant. This may be because only a few people in the study used injections (12 of 1741).
- IUD use was associated with a small reduction in ovarian cancer risk.
- This finding was not statistically significant. This may be because only a few people in the study used IUDs (64 of 1741).
- The use of implants reduced ovarian cancer risk by 70%.
Participants who did not develop ovarian cancer were more likely to:
- have breastfed their children. This is in line with other research we covered here.
- have slightly more children (on average).
- have had a tubal ligation (had their tubes tied).
Strengths and limitations
Strengths:
- Participants with ovarian cancer were matched to participants who did not have ovarian cancer, by the year they entered the study, birth year, country of residence, mutation type and breast cancer history.
- The study enrolled a large number of participants and followed them for about 20 years.
Limitations:
- Relatively few people used forms of birth control other than birth control pills. While participants who used implants, injections and IUDs to decrease risk had a lower risk for ovarian cancer, these results should be viewed with caution due to the low number of people who used these forms of birth control.
- The information on participants’ cancer history and birth control use was self-reported, so it is possible some of the information was inaccurate.
- Because the number of people who used long-acting forms of birth control was small, further study is required to assess how these contraceptives may reduce ovarian cancer risk.
Context
Using birth control pills can reduce the risk of ovarian cancer in the general population. This study shows that using birth control pills also decreases ovarian cancer risk in people with a mutation. It also offers new data that for high-risk people, birth control injections, implants and IUDs may also offer protection against ovarian cancer. However, because the number of people in this study who relied on these methods of birth control was small, more research is needed.
FORCE offers many peer support programs for people with inherited mutations.
- Our Message Boards allow people to connect with others who share their situation. Once registered, you can post on the Diagnosed With Cancer board to connect with other people who have been diagnosed.
- Our Peer Navigation Program will match you with a volunteer who shares your mutation and situation.
- Our moderated, private Facebook group allows you to connect with other community members 24/7.
- Check out our virtual and in-person support meeting calendar.
- Join one of our Zoom community group meetings.
Updated: 08/06/2022